The Importance of Immune System Dysregulation in People with Down Syndrome
From Down Syndrome World Issue 3 2018
How does an extra copy of chromosome 21 drive the developmental and clinical features of Down syndrome? This question has been the subject of many investigations since 1958, when Jérôme Lejeune reported the Presence of trisomy 21 in cells of people with Down syndrome. The answer has remained elusive.
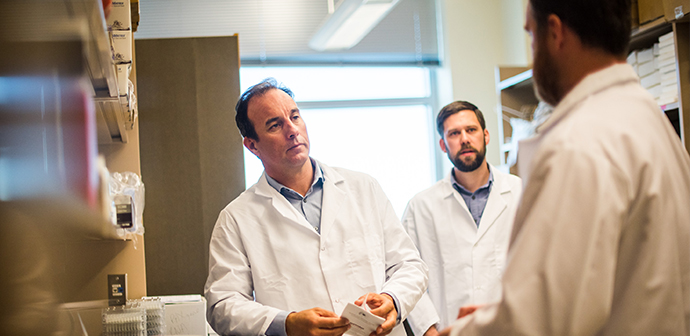
NOW, RESEARCH FROM the Linda Crnic Institute for Down Syndrome points to dysregulation of the immune system as a mechanism by which the extra chromosome would cause this multiorgan, multi-system condition. The implications of these results are profound, because they not only provide a new conceptual framework for future research, but also illuminate avenues for the development of novel diagnostic and therapeutic opportunities to improve health outcomes in Down syndrome. Of the more than 20,000 genes encoded in the human genome, chromosome 21 carries fewer than 300, the lowest number of genes on any human chromosome. While consensus among scientists is that Down syndrome is a “polygenic condition,” a condition caused by increased activity of more than one gene, it is also agreed that not all genes on chromosome 21 would contribute equally to the condition. If one were to select a random group of 300 genes, it is recognized that only a few genes would be master regulators of cellular and organismal function. What then are the master regulator genes on chromosome 21 with the greatest impact on human biology? To address this question, scientists at the Crnic Institute employed an approach known as functional genomics, which involves measurements of the activity of thousands of genes across the entire genome, to identify the gene networks most impacted by trisomy 21.
OVERACTIVE IMMUNE SYSTEMS?
The first set of results from the analysis of cells of people with Down syndrome (Sullivan et al., 2016) revealed that trisomy 21 causes constitutive activation of the gene network known as the Interferon response, a key branch of the immune system responsible for fighting off viral infections. In cells from typical people, the Interferon response was dormant, but cells from people with Down syndrome seemed to be fighting off a viral infection that just wasn’t there. These results immediately drove attention to four genes on chromosome 21 known as the Interferon receptors, which are required for cells and tissues to respond to a viral infection and whose triplication could potentially trigger constant activation of this arm of the immune system.
The second set of results from the analysis of blood samples (Sullivan et al., 2017) revealed signs of chronic autoinflammation in people with Down syndrome. Measurements of approximately 4,000 different proteins in the blood identified about 300 that are differentially abundant between people with and without Down syndrome, with about half of those 300 proteins being involved in the immune system. Importantly, this study revealed signs of both constant activation and exhaustion of different aspects of the immune system, with obvious ties to the Interferon response. It is well established that the Interferon response enhances anti-viral defenses, but too much Interferon activity eventually weakens antibacterial defenses. Indeed, the results of the blood analysis were consistent with a type of immune dysregulation caused by lifelong hyperactivation of the Interferon response.
Noteworthy, both studies revealed, among people with Down syndrome, strong inter-individual variation in the degree of activation of the Interferon response and autoinflammation, which could potentially be linked to the obvious clinical diversity in this population.
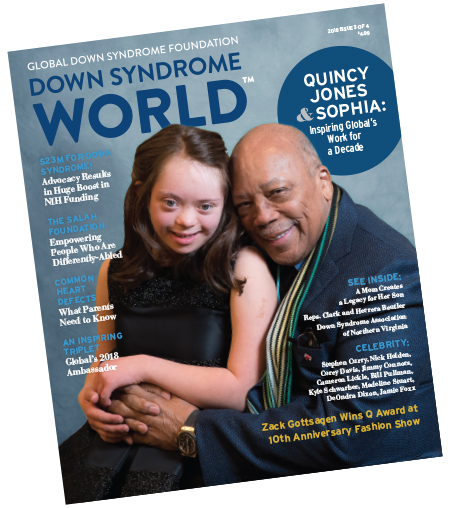 This article was published in the award-winning Down Syndrome World™ magazine. Become a member to read all the articles and get future issues delivered to your door!
This article was published in the award-winning Down Syndrome World™ magazine. Become a member to read all the articles and get future issues delivered to your door!GREATER INSIGHTS AND POTENTIAL TREATMENTS
These results have triggered a flurry of activity at the Crnic Institute to answer key follow-up questions: Which of the symptoms of Down syndrome could be explained by the observed immune dysregulation? To what degree is the immune dysregulation caused by triplication of the four Interferon receptors versus other genes on chromosome 21? What would be the diagnostic value of measuring immune dysregulation to predict the risk of the same person developing certain co-occurring diseases or conditions? What would be the therapeutic value of medications that inhibit the Interferon response and accompanying inflammatory process?
Several key facts are generating much enthusiasm in the pursuit of these answers. First, it is well established that a hyperactive Interferon response has negative effects on human development, as illustrated by type I Interferonopathies, a newly recognized class of genetic conditions caused by gene mutations that lead to activation of the Interferon response and share many symptoms with Down syndrome. Second, the pharmaceutical industry has developed many medications that inhibit the Interferon response, some of which are approved for the treatment of autoinflammatory conditions, such as rheumatoid arthritis, and are currently being tested for the treatment of autoimmune conditions more prevalent in Down syndrome, such as alopecia areata and vitiligo. Third, pioneer studies in mouse models of Down syndrome completed by Lenny Maroun, Ph.D., currently at the Crnic Institute, demonstrated that reducing the Interferon response improves the development of these mice (Maroun et al., 2000).
Altogether, this body of research justifies a strong investment in the study of the immune system in Down syndrome, with the obvious potential to develop diagnostic and therapeutic strategies to improve the well-being of those living with trisomy 21.
To learn more about research at the Crnic Institute, visit globaldownsyndrome.org/our-story/linda-crnic-institute.
References:
Maroun, L.E., Heffernan, T.N., and Hallam, D.M. Partial IFN-alpha/ beta and IFN-gamma receptor knockout trisomy 16 mouse fetuses show improved growth and cultured neuron viability. Journal of Interferon & Cytokine Research: the Official Journal of the International Society for Interferon and Cytokine Research. 2000; 20, 197–203.
Sullivan, K.D., Evans, D., Pandey, A., Hraha, T.H., Smith, K.P., Markham, N., Rachubinski, A.L., Wolter-Warmerdam, K., Hickey, F., Espinosa, J.M., et al. Trisomy 21 causes changes in the circulating proteome indicative of chronic autoinflammation. Scientific Reports. 2017; 7, 14,818.
Sullivan, K.D., Lewis, H.C., Hill, A.A., Pandey, A., Jackson, L.P., Cabral, J.M., Smith, K.P., Liggett, L.A., Gomez, E.B., Galbraith, M.D., et al. Trisomy 21 consistently activates the interferon response. 2016; eLife. 5.
Like this article? Join Global Down Syndrome Foundation’s Membership program today to receive 4 issues of the quarterly award-winning publication, plus access to 4 seasonal educational Webinar Series, and eligibility to apply for Global’s Employment and Educational Grants.
Register today at downsyndromeworld.org!
Recent Posts
- Exclusive Interview with Edmonton Down Syndrome Society Executive Director Janet Tryhuba
- Global Down Syndrome Foundation & Down Syndrome Diagnosis Network Sign Multi-Year Collaboration Agreement
- Building the Future Gala Raises $212,000 to Support Down Syndrome Advocacy and Research
- Exclusive Interview with Down Syndrome Association of Jacksonville Executive Director Debbie Revels
- GLOBAL Raises $450,000 at their AcceptAbility Gala as Celebrities & Congress Step Out for People with Down Syndrome

 Experience our inspirational and groundbreaking videos and photos. Our children and self-advocates are beautiful AND brilliant!
Experience our inspirational and groundbreaking videos and photos. Our children and self-advocates are beautiful AND brilliant! Make sure your local Representatives are on the Congressional Down Syndrome Task Force.
Make sure your local Representatives are on the Congressional Down Syndrome Task Force.